Maternal Depression: Understanding Associated Risk Factors
By Clariza Saint George, Brett Penner, and Lara Burt
MATERNAL DEPRESSION: UNDERSTANDING ASSOCIATED RISK FACTORS
Introduction
Maternal depression is a broad term that encompasses several conditions with varying onsets. The conditions associated with maternal depression are as follows: prenatal depression, which occurs during pregnancy; baby blues, with onset a week after birth; postpartum depression, whose onset can be within the first two to three months of birth; and postpartum psychosis, which begins within two to four weeks of delivery (New York Department of Health, 2015). Women experiencing maternal depression disclosed the following symptoms: increased hostility and resentment towards others, difficulty communicating, emotional distance and disinterest, and disaffection (Field, 1998; Gelfand & Teti, 1990; Lovejoy, Graczyk, O’Hare, & Neuman, 2000). A diagnosis of maternal depression, or the prominence of depressive symptoms, negatively impacts the mother’s ability to foster healthy relationships and execute management functions strongly tied to parenting (e.g., ensuring adequate nutrition) (Knitzer, Theberge, & Johnson, 2008).
Maternal depression disproportionately affects women of color (Cardoso, Padilla, & Sampson, 2010; Knitzer, Theberge, & Johnson, 2008). Compounded with the implications related to maternal depression, women of color experience unique sets of circumstances exclusively related to their race (Cardoso, Padilla, & Sampson, 2010). Research has found that women of color are more likely to report depressive symptoms when compared to others. Hispanic and African American women with lower socioeconomic status (SES) have higher rates of depressive symptoms when compared to white middle-class women (Yonkers et al., 2001). Research has found a strong positive relationship between race and ethnicity and SES as predictors of mental illness (Cardoso, Padilla, & Sampson, 2010; Knitzer, Theberge, & Johnson, 2008).
The impact of maternal depression is not limited to the mother, but rather reverberates throughout the family. An estimated 15 million children live with a mother experiencing depression (Beck, 1995; National Research Council and Institute of Medicine, 2009). The impacts of maternal depression can be felt from birth: children with depressed mothers were in lower weight percentiles when compared to children with non-depressed mothers (Field, 1998). Beyond the physiological impact, there are long-lasting, harmful effects on the psychological and physical health and well-being of a depressed mother’s children. Children whose mothers suffered from depression score high in depressive symptoms, have reduced cognitive, behavioral, and emotional functioning, and are at a higher risk of developing maladaptive social behaviors (Cardoso, Padilla, & Sampson, 2010; Field, 1998; Gelfand & Teti, 1990; Knitzer, Theberge, & Johnson, 2008; Lovejoy, Graczyk, O’Hare, & Neuman, 2000; Mistry et al., 2010). These maladaptive social behaviors include anxiety, behavioral problems, and difficulties with interpersonal communication (Cardoso, Padilla, & Sampson, 2010; Knitzer, Theberge, & Johnson, 2008).The age of the child has been found to influence the type of effect (Gelfand & Teti, 1990). Young children who spend most of the day in close proximity to their depressed mothers show difficulty with compliance and disturbances to attachment and attention (Gelfand & Teti, 1990). School age children face similar difficulties, along with trouble building relationships with teachers and peers as well as lower school achievement (Gelfand & Teti, 1990). The most pronounced impact of maternal depression on children is the occurrence of psychological disorders in the child later in life: an increased risk for psychopathology including conduct, mood, and affective disorders (Gelfand & Teti, 1990).
Our study therefore seeks to understand the factors that contribute to maternal depression, focusing on work stress and income level. The goal of the study was to determine the impact of work stress and income level independently and together. The decision to explore these two variables is based on the extensive literature that demonstrates a positive correlation between poverty and cognitive development (Petterson & Albers, 2001). Successful prevention and treatment of maternal depression requires an awareness of the many risk factors tied to the condition. Given that research has shown that maternal depression is a variable in child outcomes as early as birth, we believe the findings of our study make an important contribution to policies impacting early childhood care. Recognition of these risks factors for maternal depression could result in improved outcomes for the mother, her children, and the entire family (Gelfand & Teti, 1990; Yonkers, Vigod, & Ross, 2011). Improving healthcare for mothers experiencing depression, and mothers in general, will benefit children and the family as a whole. Our research questions are: 1) Does parental work stress impact maternal depression? 2) Does income impact maternal depression? 3) Does parental work stress and income impact maternal depression? Our first hypothesis is that there will be a positive association between the level of parental work stress and maternal depression, i.e. as parental work stress increases so will the level of maternal depression. Our second hypothesis is that income and maternal depression will be negatively associated: as income decreases, maternal depression increases. Finally, our third hypothesis is that together, the variables of income and parental work stress will have a higher impact on maternal depression than either one of the variables alone.
METHOD
Participants
We draw on published data collected by Marshall, Roberts, and Wagner Robeson (2013) for the Massachusetts Early Care and Education and School Readiness Study. Our study uses children from two samples. The first group was made up of 170 children who are attending childcare centers and who have been followed since infancy (the Family Income, Infant Child Care, and Child Development Study). Questionnaires were mailed to the families in this study. The second group was made up of 242 children who were attending childcare centers primarily serving low-income families. For the second group of children, data was collected at 12 months, 24 months, and pre-kindergarten; questionnaires were again sent in the mail. Of the 373 children used in the study, 144 reported being female, 56 reported being male and 73 did not report their gender. The ethnicities of the children in the study were as follows: 5.4% (n = 20) Native American, 14.5% (n = 54) Asian, 46.1% (n = 172) Black, Other 10.5% (n = 39), and Hispanic 4.0% (n = 15). Ethnicity data was missing for 19.6% (n = 73) of the children in the study.
Measures
Maternal depression
The dependent variable in our study was maternal depression. Maternal depression is a continuous variable: a higher score equals more depression. In order to measure this variable, the study used the Center for Epidemiologic Studies Depression Scale (CES-D), which measures symptoms defined by the DSM-V (American Psychiatric Association, 2013).
Socio-economic status
As a measure of socioeconomic status, we used the variable household income at 48 months/pre-K This input is nominal, and we divided it into two categories: lower than $40,000 and greater than $40,000. These categories emerged from trends noticed during the graphing of income levels and the income level that is said to mark lower middle class in Massachusetts ($44,512), a value that supported the two categories used in the data analysis (Feinauer, 2015).
Work stress
We looked at parental work stress as our second independent variable. Similar to maternal depression, this variable is also continuous: the higher the score the more work stress. Working mothers experience a unique set of circumstances as they navigate home life and the workforce. Negative emotion spillover is defined as feelings of anger, frustration, and disappointment at work creating issues at home (e.g., power assertion, irritability, or impatience), contributing significantly to an individual’s stress level (Goodman & Crouter, 2009; Repetti & Wood, 1997). Workplace stressors range in their type and severity. They include lack of time f lexibility, high levels of pressure, excessive workloads, conflict with colleagues, and a lack of control over labor (Goodman & Crouter, 2009; Repetti & Wood, 1997).
As previously mentioned, numerous work stressors have been linked to the prominence of depressive symptoms and a depression diagnosis in working parents (Goodman & Crouter, 2009). Thomas and Ganster (1995) found that working mothers with children younger than 16 with inf lexible work schedules reported higher depression levels (as cited in Goodman & Crouter, 2009). The lack of a working mother’s ability to create a f lexible work schedule makes it significantly more difficult for her to balance her home and work responsibilities. The frustration created by the inability to adequately create a balanced home and work schedule negatively affects the parent’s caregiving ability. For example, research from Brody et al. (1994) found that parents who report higher dissatisfaction with their employment implement more coercive parenting styles and harsher punishments at home compared to parents who did not (as cited in Raver, 2003). Mothers who use stringent parenting tactics reported higher depressive symptoms, increased irritability, and stronger feelings of pessimism; this combination yielded an overall decline in their caregiving quality (Goodman & Crouter, 2009; Raver, 2003).
Income level
The rate of low-income women with the diagnosis of depression or depressive symptoms is higher than that of women with higher income levels (Cardoso, Padilla, & Sampson, 2010; Currie, 2005; Knitzer, Theberge, & Johnson, 2008). Knitzer, Theberge, and Johnson (2008) found that 25% of low-income women experience depression or depressive symptoms in a given year (Currie, 2005; Knitzer, Theberge, & Johnson, 2008). Depression is a complex diagnosis; it is able to manifest itself as physical ailments and therefore can negatively impact one’s physical ability to work. According to Zill et al. (1995), mothers with menial, low-paying, and low-skill jobs reported more negative effects than mothers with higher-paying and better quality positions (as cited in Raver, 2003).
RESULTS
Descriptive Statistics
For the 373 participants, mean maternal depression scores were 8.99 (SD 8.56). The minimum score reported was 0.00, and the maximum was 47.00. Scores of 3, 6, and 13 represented the 25th, 50th, and 75th percentiles, respectively. For the income variable, 34.9% of respondents had an income of lower than $40,000, 65.1% reported an income greater than $40,000, and 22.5% of respondents did not answer the income question. Parental work stress had a mean score of 19.63 (SD = 6.45). Scores of 15, 19, and 23 represented the 25th, 50th, and 75th percentiles, respectively.
Correlation analysis
To determine whether increases in parental stress were associated with increases in maternal depression symptoms, we performed a correlation analysis. This analysis, summarized in Table 1, revealed two significant correlations. Parental work stress and maternal depression were significantly positively correlated, but the strength was relatively weak, r(269) = 0.345. In addition, income and work stress were significantly negatively correlated, and this association was also relatively weak, r(269) = -0.265 (Table 1). The correlation between income and work stress did not yield a significant result.
Table 1
Correlation Table
| Score for Maternal Depression | Score For Parent Work Stress | Income (Bivariate) | |
| Score for Maternal Depression | 1 | 0.345** | -2.65*** |
| Score for Parent Work Stress | 0.345** | 1 | -0.121 |
| Income (Bivariate) | -0.265** | -0.121 | 1 |
Note: ** p 0.01; *** p 0.001
Simple Linear Regression
A simple linear regression was used to predict changes in maternal depression by work stress and income individually. The regression for work stress, summarized in Table 2, indicated that 11.6% of the variation in maternal depression is explained by income, (F(1, 267) = 36.133, P < 0.000). As parental work stress increases by 1 standard deviation, maternal depression increases by 0.345 standard deviations.
Table 2
Linear Regression Work Stress on Maternal Depression
| Variable | B | SE B | β | t | sig. |
| Score for Parent Work Stress | 0.465 | 0.77 | 0.345 | 6.011 | 0.000*** |
Note: Adj. R2 = 0.116; *** p 0.001
The same analysis was also performed for the influence of income on maternal depression: 6.7% of the variation in maternal depression can be explained by income, (F(1, 287) = 21.67, p < 0.000). As income increases from the low to high-income category, maternal depression decreases by 0.265 standard deviations. This analysis is summarized in Table 3 below.
Table 3
Linear Regression Bivariate Income on Maternal Depression
| Variable | B | SE B | β | t | sig. |
| Bivariate Income | -4.75 | 1.021 | -0.265 | -4.655 | 0.000*** |
Note: Adj. R2 = 0.067; *** p 0.001
Multiple Regression
To understand how the variables influence maternal depression when considered together, a multiple regression analysis was performed (Table 4). These variables explain 16.3% of the variation in maternal depression, (F(2,257) = 26.129). Consistent with the results reported above, parent work stress provided positive weight to the model, indicating that those with higher work stress levels can be expected to have higher maternal depression levels. Income, conversely, provided negative weight to the model; higher income is associated with lower maternal depression. Both income and work stress were significant predictors of maternal depression at the 0.001 level.
Table 4
Multiple Linear Regression of Income and Work Stress on Maternal
| Variable | B | SE B | β | t | sig. |
| Score for Parent Work Stress | 0.462 | 0.77 | 0.319 | 5.564 | 0.000*** |
| Bivariate Income | -4.116 | 1.054 | -2.24 | -3.097 | 0.000*** |
Note: Adj. R2 = 0.163; *** p 0.001
FINDINGS
Our results support our hypothesis that parental work stress and maternal depression are positively associated. Findings demonstrated that as work stress increases, so does maternal depression. However, the explanatory power of work stress was not as high as expected. The adjusted R2 indicated that only a minor portion of the variation in maternal depression is explained by work stress. This finding appears in line with the correlation coefficient between the two variables as a relatively weak correlation of 0.345 was found. Although the relationship was relatively weak, the significance level of p < 0.001 indicates that it is highly unlikely that the observed differences between work stress and maternal depression are due to chance. This finding supports the existing literature on stress and depression. Goodman and Crouter’s (2009) theory of negative emotional spillover and Thomas and Ganster’s (1995) finding of higher depression levels among working mothers with young children are supported by these findings and can help explain why the p-value was so low.
The results on income and maternal depression also supported our hypothesized relationship between the variables. The simple linear regression indicated that a negative relationship exists between income and depression: as income increases maternal depression decreases. This relationship was significant at the p < 0.001 levels Thus, the null hypothesis is rejected; there is a relationship between income and maternal depression. However, much is left unexplained by this analysis. As the correlation coefficient indicates, the relationship between these variables is very weak, only -0.265. Moreover, the R2 indicates that only 6.7% of the variation in stress is explained by income alone.
It was hypothesized that the effect of income would be mediated according to work stress. A high income and high-stress job is likely to have a different effect on depression than a high-income job with low stress. However, a correlation matrix revealed no significant relationship between work stress and income, indicating that no interaction between work stress and income exists, highlighting the need to consider income along with other factors. It should also be noted that variables such as work benefits and financial aid for care were not included in this analysis. Expanding our operationalization of socioeconomic status (SES) to include these factors might lead to a different result.
The shortcomings discussed with the income model support our third research question of the effect of work stress and income together on depression. In this model, the explanatory power of the variables increased to 16.3 percent. In addition, the absolute value of the t-values indicates that work stress contributes greater weight to the model. Both p-values were significant at the p <.001 levels, allowing for the rejection of the null hypothesis. A relationship exists between work stress, income, and maternal depression.
Figure 1 plots the effect of work stress on maternal depression by income category. This graph further confirms there is no clear relationship between work stress and income. The highest level of maternal depression was reported from those who have low income, medium stress jobs. Among the majority of the work stress scores, depression is highest when income is in the lower category. However, in the present data there are several exceptions to this finding precluding the ability to draw a relationship between work stress and income.
Overall, the R2 of 0.163 implies that much is missing from the model. While the data confirm the hypothesized relationships between the data, it can only be concluded that work stress and income have a significant but small effect on maternal depression. The aim of this research was to investigate the effect of work stress and SES on maternal depression. Although this aim was accomplished, the analysis raises other questions as well. These questions, along with other limitations of this study, will be discussed in the following sections.
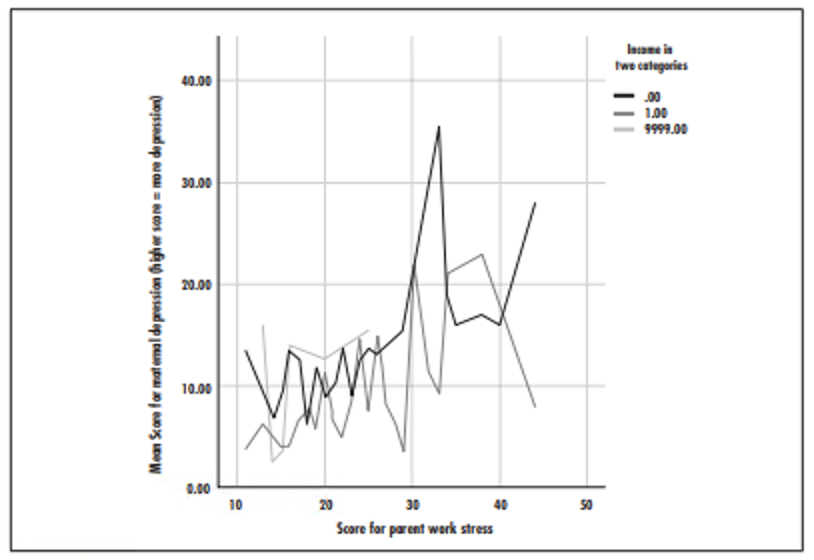
Figure 1. Histogram of maternal depression scores related to parental work stress and income as a dichotomous variable.
Limitations
The goal of this report was to re-examine maternal depression and discern whether work stress is positively correlated with it, and also whether work stress and SES impact maternal depression. Current literature involving work stress and parental caregiving does not examine these factors. With the hope of filling the present gap, this study neglected to inspect other variables that may impact maternal depression with regard to work stress and SES. The literature review revealed that other academics found a positive relationship between SES and race when maternal depression was examined. Future researchers should consider using an ethnographic approach to inform which variables are essential for the regression analyses.
The sample size for each of the three variables explored was different. Twenty-two percent of respondents did not respond when prompted about their income. A total of 373 individuals participated in this study. Only 300 participants provided a response to the question about maternal depression; 269 responded to the parent work stress questions; and 289 reported their income range. Our sample size was thus 269. The reporting discrepancies make it difficult for a complete picture to be generated and analyzed.
The income variable that was explored in the present study was very limited and did not include other sources of income, such as alimony, child support, food stamps, cash-assistance, and other forms of supplemental income. The participants reported their income when their child was 48 months old/before kindergarten and not at other crucial junctures during the child’s development. Parental marital/relationship status and education level are also important factors related to a family's income. Changes to relationship status may impact the amount of income the family has on a monthly basis.
The workplace benefits variable did not encompass the totality of benefits that may have been offered by employers, such as child care assistance, maternity/paternity leave, sufficient health care benefits, and f lexible work scheduling. Foregoing to include important aspects related to workplace benefits severely impacted this study’s ability to calculate its effect when combined with income. In addition, workplace benefits are limited to those of the workplace and do not include educational institutions such as college, graduate school, or trade programs. Historically, these institutions offer assistance to their students in the form of financial aid, independent study, full-time/part-time options, night classes, and even child care.
Finally, the variables inspected in this study—maternal depression, parental work stress, and income range—were not operationally defined. Due to this, the respondents most likely used their personal understanding of these abstract and broad terms. Using a subjective rather than objective definition of these crucial variables has limited this data set’s ability to be extrapolated onto the general public. Reduction in the generalizability of these analyses is a large limitation. The lack of defined key terms combined with varying sample sizes and incomplete variables did not allow for the entirety of the concluded correlations to be explored. Suffice to say, although statistical significance was yielded in both models, the data set was relatively incomplete and may not be easy to translate to large populations.
CONCLUSION
The aim of this research was to demonstrate the effects of workplace stress and socioeconomic status on maternal depression. Results indicate that both variables are significant predictors of depression levels. Significant relationships were found when each explanatory variable was considered alone, as well as when they were considered together in a multiple regression analysis. P-values for all analysis were less than 0.001, highlighting the improbability of these relationships being due to chance. However, the R2 numbers of each of the models were not as high as expected, indicating the need for future research. The multiple regression R2 was only 0.163, indicating that much of the explanation for changes in maternal depression remains missing. It is suggested that a qualitative study be conducted to solicit ideas on the influencers of maternal depression, leading to the construction of a more powerful model. Overall, while there is room for improvement, this study demonstrates an important step in examining the link between workplace stress, socioeconomic status, and depression.
It is our hope that this study can lead to improvements in the screening and treatment of maternal depression. As previously mentioned, the impact of this diagnosis is not limited to the mother. It has substantially detrimental effects on the child, ranging from difficulty building relationships to stunted academic growth. Creating social and organizational policies to improve individual and familial outcomes resulting from maternal depression may reduce the likelihood and severity of cognitive, psychological, and physical impacts. Although determining the exact remedy to this pervasive disorder is not within the purview of the authors, we suggest simple and relatively inexpensive interventions that require minimal effort. Postpartum depression screening tools are in abundance and have been shown to be effective tools in evaluating the presence of depression or anxiety symptoms (American College of Obstetricians and Gynecologists, 2008). This study identified a positive relationship between parental work stress and maternal depression and a negative relationship between income level and maternal depression; the combination of income and parental work stress has a more significant impact on maternal depression than each on their own.
REFERENCES
American College of Obstetricians and Gynecologists. (2008). Perinatal depression screening tools for obstetrician-gynecologists. American College of Obstetricians and Gynecologists. Retrieved from http://mail.ny.acog.org/website/DepressionToolKit.pdf.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Beck, C. T. (1995). The effects of postpartum depression on maternal-infant interaction. Nursing Research, 44(5), 298-304. doi:10.1097/00006199-199509000-00007
Cardoso, J. B., Padilla, Y. C., & Sampson, M. (2010). Racial and ethnic variation in the predictors of maternal parenting stress. Journal of Social Service Research, 36(5), 429-444. doi:10.1080/01488376.2010.510948
Currie, J. M. (2005). Health disparities and gaps in school readiness. The Future of Children, 15(1), 117-138. doi:10.1353/foc.2005.0002
Feinauer, J. J. (2015, April 21). What it takes to be middle class in each state. Deseret News. Retrieved from http://www.deseretnews.com/top/3184/18/Illinois-What-it-takes-to-be-middle-class-in-each-state.html.
Field, T. (1998). Maternal depression effects on infants and early interventions. Preventive Medicine, 27(2), 200-203.
Gelfand, D. M., & Teti, D. M. (1990). The effects of maternal depression on children. Clinical Psychology Review, 10(3), 329-353.
Goodman, W. B., & Crouter, A. C. (2009). Longitudinal associations between maternal work stress, negative work-family spillover, and depressive symptoms. Family Relations, 58(3), 245-258. doi:10.1111/j.1741-3729.2009.00550.x
Knitzer, J., Theberge, S., & Johnson, K. (2008). Reducing maternal depression and its impact on young children: Toward a responsive early childhood policy framework. National Center for Children in Poverty. Retrieved from http://www.nccp.org/publications/pdf/text_791.pdf.
Lovejoy, M., Graczyk, P. A., O'Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior. Clinical Psychology Review, 20(5), 561-592. doi:10.1016/s0272-7358(98)00100-7
Marshall, N., Roberts, J., & Wagner Robeson, W. (2013). Massachusetts early care and education and school readiness study, 2001-2008. ICPSR33968-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2013-03-28. http://doi.org/10.3886/ICPSR33968.v1
Mistry R. S., et al. (2010). Family and social risk, and parental investments during the early childhood years as predictors of low-income children’s school readiness outcomes. Early Childhood Research Quarterly, 25: 432–449.
National Research Council and Institute of Medicine. (2009). Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: The National Academies Press.
New York Department of Health. (2015, January). What is maternal depression? Retrieved from https://www.health.ny.gov/community/pregnancy/health_care/perinatal/maternal_depression/providers/what_is_maternial_depression.htm
Petterson, S. M., & Albers, A. B. (2001). Effects of poverty and maternal depression on early child development. Child development, 72(6), 1794-1813.
Raver, C. C. (2003). Does work pay psychologically as well as economically? The role of employment in predicting depressive symptoms and parenting among low-income families. Child Development, 74(6), 1720-1736 doi:10.1046/j.1467- 8624.2003.00634.x
Repetti, R. L., & Wood, J. (1997). Effects of daily stress at work on mothers' interactions with preschoolers. Journal of Family Psychology, 11(1), 90-108. doi:10.1037//0893- 3200.11.1.90
Yonkers, K. A., Ramin, S. M., Rush, A. J., Navarrete, C. A., Carmody, T., March, D., . . . Leveno, K. J. (2001). Onset and persistence of postpartum depression in an inner-city maternal health clinic system. American Journal of Psychiatry, 158(11), 1856-1863. doi:10.1176/appi.ajp.158.11.1856
Yonkers, K. A., Vigod, S., & Ross, L. E. (2011). Diagnosis, pathophysiology, and management of mood disorders in pregnant and postpartum women. Obstetrics & Gynecology, 117(4), 961-977.
CLARIZA SAINT GEORGE is a clinical student at the School of Social Service Administration in the Alcohol and Other Drug Abuse program of study; she will be graduating in 2017. She graduated with honors in 2014 from Northeastern Illinois University where she received her B.A. in psychology with a minor in women and gender studies. Her past publications include: The Etiology of Intravenous Heroin Use in Adolescent Girls (2016). Her academic interests include: interpersonal violence, substance use, LGBTQIA+, and PLWHA.
BRETT PENNER is a second-year administration student at the school of Social Service Administration, with a concentration in policy planning, analysis, and advocacy. His interests center on housing issues, primarily the work to create public policies that lead to better housing outcomes. He currently interns at Corporation for Supportive Housing, where he aids state efforts in advocating for access to housing for underserved populations. Prior to attending SSA, Brett served as an AmeriCorps member at Franciscan Outreach in Chicago. Brett holds a B.A. in sociology from the University of Illinois at Urbana-Champaign.
LARA BURT is a second-year administration student participating in the Family Support program of study attheSchool of Social Service Administration. She currently interns at Youth and Opportunity United in Evanston, where she works with the community schools team supporting a parent leadership group, as well as in program development and evaluation. Prior to coming to SSA, Lara worked as a Metro DC Reading Corps tutor in Washington, D.C., providing individualized reading instruction to students in grades K-3. Lara holds a B.A. in international relations and German from the University of Michigan.